Table of Contents
What is food poisoning?
Food poisoning is a common acute condition where food or water contaminated with infectious agents causes inflammation of the gut. These infectious agents may be viruses, bacteria, protozoa or their toxins. Unlike with the ‘stomach flu’ (viral gastroenteritis) which is caused by viruses, food poisoning is more commonly caused by bacteria like E.coli, Salmonella and Shigella.
Once the bacteria enter the gut it causes inflammation and damage to the wall of the gut. This causes symptoms like nausea, vomiting, abdominal pain or cramps and diarrhea. Food poisoning is acute. It arises suddenly, within minutes to hours after consuming contaminated food or water and resolves within a few days. Medication like antibiotics may be necessary but sometimes supportive measures like bed rest and rehydration will suffice.
Causes of Food Poisoning
Bacteria that can cause diarrhea in human live in the intestines of healthy or infected people, or animals, like cattle, poultry or pets. Their stool may contaminate drinking or recreational water, soil, vegetables on fields, milk during milking, meat during slaughter, or food prepared with the hands contaminated with stool. Beside that, bacteria arising from the air or food storing surfaces may quickly multiply in a non-cooled food.
Sources of Infection:
- Food borne infection (food poisoning): undercooked ground beef (hamburgers), chicken or other meat, shellfish (oyster, scallops), raw eggs (mayonnaise), raw unwashed fruits and vegetables, unpasteurized milk or fruit juices, or non-adequately stored or cooled food
- Water borne infection: contaminated drinking or recreational water
- Stool-to-mouth (fecal-oral) infection via stool-contaminated hands, toys, utensils, soil, etc.
- Infections of ear, nose and throat, and urinary infections may also cause acute bacterial diarrhea.
Bacteria, Commonly Involved in Food Poisoning
- E.coli 0157:H (2)
- Campylobacter (3)
- Salmonella (4)
- Staphylococcus aureus (staph food poisoning)
- Clostridium perfringens
- Shigella (5,6)
- Listeria – in pregnant women and persons with lowered immunity (7)
- Yersinia
- Vibrio cholerae (causing cholera)
Intestinal Changes in Bacterial Food Poisoning
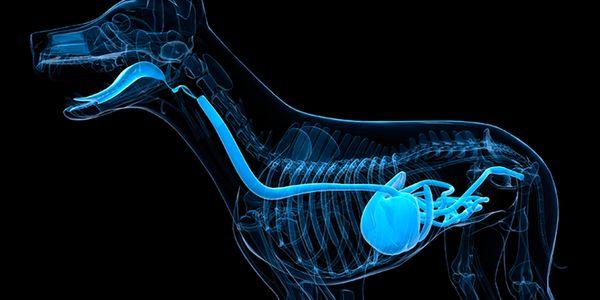
Bacteria may cause inflammation of the stomach and small intestine (gastroenteritis), colon (colitis) or rectum (proctitis). Inflammation may lead to reduced absorption of nutrients and water from the intestine resulting in diarrhea. In heavy infection ulcers may develop, and in most severe cases bacteria may enter the blood (sepsis) and affect other organs.
Symptoms of Bacterial Food Poisoning
Symptoms of food poisoning caused by bacteria include:
- Explosive diarrhea with frequent, loose or watery stools, urgency, bloating, abdominal cramps. If enough bacteria are ingested, diarrhea appears suddenly, usually within 48 hours (or within 5 days), and lasts for 1-3 days (or up to 10 days or more in heavy infection).
- Nausea, vomiting (occasionally)
- General malaise with fever (occasionally)
- In severe diarrhea, symptoms of dehydration, like thirst, tiredness, sunken eyes, low amount of morning urine, may quickly appear
If you have persistent diarrhea or soft stools after a travel, read about traveler’s diarrhea and intestinal parasites, like Giardia and intestinal worms contracted by food.
The stool of the infected person is contagious during diarrhea and up to two weeks after the healing (in shigellosis possibly up to 1 year or more after symptoms cessation).
Diagnosis of Bacterial Food Poisoning
Doctor can suspect you have bacterial food poisoning from the history of
- Sudden onset diarrhea
- Diarrhea appearing several hours after eating fastfood, having a meal in a suspicious restaurant or drinking water from rivers or lakes
- Other people who have eaten the same food as you and had diarrhea within the next two days
- Close contact with people having diarrhea
- Arriving from a country with good hygiene into country with poor hygiene habits.
If you have severe diarrhea, a doctor might order a stool culture test to determine causing bacteria to be able to prescribe you an appropriate antibiotic. Hemoccult, test for occult blood in the stool, is done when intestinal bleeding is suspected.
Treatment of Diarrhea Due to Bacterial Food Poisoning
Mild acute bacterial diarrhea usually resolves on its own within two to three days. Rehydration is essential to prevent complications. Water alone is not sufficient and oral rehydrating solutions need to be used to ensure the optimal concentration of electrolytes is administered and replaced. If dehydration is severe or a person cannot hold down fluid orally, then intravenous rehydration is necessary.
Antibiotics are prescribed only in prolonged (>5 days), profuse (>6 stools/day) or bloody diarrhea, with a high fever (> 38.5 °C or 101.3 °F), or severe abdominal pain. It is important that antibiotics are prescribed by a medical professional and that the entire course is completed as advised. Antibiotics may shorten the course of severe bacterial diarrhea if the bacteria are directly involved.
However, antibiotics may have limited benefit in cases where the toxins are responsible for the illness, as may be the case with E.coli 0157:H, Staphylococcus aureus, or Clostridium perfringens. Instead the toxins need to be flushed out of the system. This is one of the reasons that antidiarrheal agents like loperamide is not prescribed immediately for food poisoning. Sometimes activated charcoal may be prescribed to help neutralize these toxins.
Remedies in Food Poisoning
Antidiarrheal medication, like loperamide, diphenoxylate, bismuth sub-salycilate, are of limited value and can worsen the diarrheal illness if used very early (1). Therefore it is important to not stop the diarrhea as it is just a symptoms. Treatment must be directed at the underlying cause which is either the presence of the bacteria or toxins in the gut, as is the case with antibiotic use.
Conservative measures should focus on rest and recovery, restoring the normal intestinal flora (“good bowel bacteria”) and preventing dehydration. The following dietary and lifestyle remedies may therefore be helpful:
- Ensure adequate electrolyte and fluid replenishment with oral rehydrating solutions (ORS). If a suitable commercial ORS is not available, then a home made solution can be prepared using 2 liters (68 ounces) of clean water, 8 teaspoons of sugar and one quarter teaspoon of table salt.
- Use a suitable probiotic as advised by a doctor or pharmacist. Avoid live culture dairy like yogurt as the lactose (milk sugar) can worsen diarrhea. This is due to secondary lactose intolerance that arises temporarily in some cases of severe diarrheal illnesses.
- Get plenty of rest and preferably strict bed rest. This helps limit dehydration that can occur with physical activity and avoid straining the body further.
Complications of Food Poisoning
Rarely, diarrhea caused by bacterial food poisoning may be accompanied or followed by nose bleeding, body swelling, painful joints, muscle paralysis due to exaggerated body reaction to harmful bacteria.
Hemolytic Uremic Syndrome (HUS)
Hemolytic uremic syndrome (HUS) may appear in children having diarrhea caused by food poisoning with Escherichia coli 0157:H7 or other bacteria. From the intestine, bacteria may enter the blood and break down red blood cells (hemolysis) that clog kidney vessels what may result in kidney failure. (Uremia refers to increased blood urea (a product of protein breakdown), which can not be successfully removed by impaired kidneys, so it builds up in the blood).
Symptoms of HUS include: nose bleeding, pale skin with bruises, profound fatigue, fever, swelling of the face or limbs and decreased urination or blood in the urine usually develop several days after the start of diarrhea, mostly in children under 10 years of age.
A child with the mentioned symptoms has to be admitted to hospital promptly. Diagnosis is made by blood test that reveal low level of red cells and platelets, and presence of bacteria. Treatment with blood transfusion and kidney dialysis usually results in full recovery (1). Without proper treatment, permanent kidney damage or even death may occur.
Reactive Arthritis (Reiter’s Syndrome)
Reactive arthritis may appear 1-3 weeks after start of diarrhea due to food poisoning with salmonella, shigella or other bacteria as:
- Painful knees, ankles and feet (arthritis)
- Burning red eyes (conjunctivitis)
- Skin rash
- Mouth ulcers
- Fever, weight loss
Symptoms may last from 3 to 12 months. Diagnosis is confirmed by blood tests (elevated sedimentation rate, bacteria, HLA B-27 markers), stool tests (bacteria) and X-ray of affected joints (2). Treatment by non-steroid anti-inflammatory drugs (Advil, Motrin), corticosteroids, antibiotics and physical therapy usually results in full recovery in few months. Disorder may reoccur, supposedly due to subsequent infection.
Guillain-Bar Syndrome
Rarely, few weeks to months after food poisoning, antibodies that attack microorganisms also cause inflammation of nerves. Weakness, numbness, painful muscle cramps or paralysis, starting in feet or arms and traveling toward the upper body, develop in some weeks and then slowly fade away in the opposite direction. Sometimes symptoms start in the head. Vision, breathing, or urination may also be affected and artificial respiration may be needed.
Occasionally, the syndrome fully develops in only few hours. Diagnosis is made from the history of diarrhea followed by neurological symptoms (when neurological symptoms appear, diarrhea is usually already healed). There is no known treatment, but plasma exchange or intravenous immunoglobulins may speed up recovery. Patients usually survive without any consequences, even in severe cases.